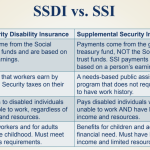
Many people believe that anyone who qualifies for Social Security Disability Insurance (SSDI or SSI) benefit payments is eligible for some immediate health insurance coverage. Unfortunately, that is not the case. In this blog post, we’ll cover who receives healthcare insurance under SSDI or Supplemental Security Income (SSI), and when each person can expect to be covered.
At Scully Disability, we’ve been providing specialized legal care to northwest Indiana’s and Chicagoland’s disabled SSDI and SSI claimants for over 35 years. Our SSDI lawyers will guide you through the entire SSDI or SSI application process and fight to win you the maximum benefits possible. We are here to answer all your questions and provide you with a free case review. Contact Scully Disability today.
Health Insurance Coverage for SSDI Recipients
Medicare health insurance coverage is available to SSDI recipients beginning 24 months after their disability onset date (DOD) when their entitlement to cash benefits began. The two-year waiting period was implemented to save the Medicare Trust Fund from what were deemed excessive costs that the fund would not be able to sustain. The long waiting period was intended to reserve Medicare coverage only to those SSD recipients whose disabilities were severe and long-lasting.
The theory that most disabled workers receiving SSDI payments could access other health insurance coverage may have been naïve and short-sighted because many self-employed workers have no health coverage through their employers and can’t qualify for Medicaid because they don’t meet the household income or financial resource limitations. This remains a serious problem for SSDI recipients who have too much income to qualify for Medicaid but far too little income to afford desperately needed medical and rehabilitative care.
Exceptions Who Don’t Wait 24 Months for Medicare Coverage
There are two exceptions to the 24-month Medicare waiting period. They are people suffering from amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s Disease, or end-stage renal disease (ESRD). Those who have ALS are enrolled in Medicare in the first month of SSDI benefits, and those with ESRD are enrolled immediately after they receive three months of dialysis treatment.
Other Insurance Available During 24-Month Waiting Period
Without Medicare coverage for the first 24 months of an SSD recipient’s benefits eligibility period, what health insurance coverage is available?
Supplemental Security Income & Medicaid: Although Medicare is not available to most SSDI recipients until after the 24-month waiting period, those SSDI recipients who also qualify for Supplemental Security Income (SSI) benefits will qualify for Medicaid coverage immediately. Unlike SSDI, which has no limitation on how many financial resources a recipient can have available, SSI is a needs-based benefit program designed to help low-income disabled individuals with few if any financial resources.
In 2022, SSI limits an individual recipient’s income to $841 per month. The income limit for couples and those with eligible dependents can be found by clicking this link. Eligibility for SSI also requires that the applicant have no more than $2,000 of countable financial resources ($3,000 for a couple). Any SSDI claimant who is eligible should apply for SSI as soon as possible to gain immediate access to Medicaid coverage for medical and healthcare costs.
Worker’s Compensation: Only disabled workers or former workers qualify for SSD benefits. Many claimants are living with work-related injury or illness allowing them to claim worker’s compensation benefits. Those who are eligible for worker’s comp will have their work-related injury and illness medical costs paid by their employer’s insurer. However, worker’s compensation laws generally do not require worker’s compensation insurers to pay medical costs for non-work-related illnesses or injuries.
It is important to remember that SSD applicants can collect worker’s compensation benefits while waiting for their SSD claim to be processed and may continue to do so even with SSD payments, though the combined benefit payments will be limited to 80% of the recipient’s usual earnings.
Cobra Continued Coverage: Many employers will continue health insurance coverage for disabled workers, but the law does not require them to do so. Instead, the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) included a provision requiring employer group health plans to offer covered workers an opportunity to continue their coverage by paying the premium entirely by themselves for a period of time. The cost is high since the employer is no longer contributing, but group health premiums are often less expensive than the alternative, individual policies.
Affordable Care Act (ACA) Marketplace: If an SSDI recipient is not eligible for the above-listed coverage options during their 24-month Medicare waiting period, then they may find a relatively low-cost insurance coverage available through their state’s healthcare.gov website.